The government’s plans for general practice will do little to improve patient access
Rishi Sunak's plan for general practice is welcome, but it will remain difficult for patients to access the service.

Stuart Hoddinott says Rishi Sunak's plan for general practice is welcome, but it will remain difficult for patients to access the service unless the government addresses long-term workforce problems
With patient 18 https://www.instituteforgovernment.org.uk/performance-tracker-2022-23/general-practice and public 19 https://www.kingsfund.org.uk/publications/public-satisfaction-nhs-and-social-care-2022 satisfaction with general practice at the lowest level on record, the government has responded with a new “Delivery plan for recovering access to primary care”. It sets out measures such as improved triage and telephony systems, increased powers for pharmacists, and a reduced set of targets.
Some of this will be welcomed by the service but, at a time of increasing demand and declining GP numbers, this plan will do little to make it easier for patients to access the care they need.
Elements of this plan will improve patient experience
Investing in a better telephony system and increased training for reception staff makes sense: patients will be more able to speak to surgery staff while receptionists will help relieve pressure on GPs.
The decision to expand the range of services that pharmacists can deliver is also sensible. There is no reason why a GP should have to take someone’s blood pressure, and the government estimates that allowing pharmacists to perform such tasks will free up 15 million GP appointments over 2023/24 and 2024/25. 20 https://www.gov.uk/government/news/what-the-prime-ministers-primary-care-recovery-plan-means-for-you It is difficult to evaluate this claim but, if true, it represents 4.6% of appointments that GPs delivered in 2022/23.
But there are also shortcomings in the plan. On the ‘front door’ interventions: an improved telephone queuing system will not reduce the size of the queue and may in fact lead to an increase as people will no longer be deterred by endless busy tones. This is a good outcome, but it will not reduce demand in the way the government hopes. On the improved triaging process: further training for practice staff will require time and management from GPs as it is rolled out. So while it may save time in the long run, it could increase GP workloads in the short term.
Finally, the government is making no new money available for any of these interventions, choosing instead to “retarget” £1 billion. This means that the government is taking money away from another part of the health system, potentially within primary care itself.
It is hard to assess the impact of additional primary care staff
Shifting work to pharmacists has been NHS policy since at least the 2014 NHS Five Year Forward View. 22 https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf , p.21 Since 2019, the government has been incredibly successful at recruiting what it calls “Direct Patient Care” (DPC) staff – in other words non-GP staff that work in primary care, of which pharmacists are one group – as part of the “Additional Role Reimbursement Scheme” (ARRS). By December 2022 the government had recruited 25.3k DPC staff –compared to its target of 26k by March 2025 – of which 5.7k were pharmacists.
But it is still difficult to assess the impact these extra staff actually have on GP workloads. There is no data about the number of procedures or appointments carried out by DPC staff specifically and GPs actually delivered more appointments than ever – even as the numbers of DPC staff tripled. There is also evidence that increased numbers of DPC staff actually adds to GP workloads, as they require more management by GPs. 26 https://www.kingsfund.org.uk/sites/default/files/2022-02/Integrating%20additional%20roles%20in%20general%20practice%20report%28web%29.pdf , p.28
The government also talks of shifting demand from one part of primary care to another, without discussing whether moving 15 million appointments onto pharmacists in the next two years is feasible. If pharmacists can absorb that much extra work easily, it is legitimate to question why they have so much spare capacity. If they cannot take on the extra appointments, then the government risks increasing pharmacists’ workloads to an unsustainable level, replicating the burnout problem that GPs are currently facing.
Increasing the number of pharmacists in primary care also has implications for the rest of the health care system: on the same day that the government released its plan to shift additional workload onto PCN pharmacists, the BBC reported that community pharmacists were closing due to a lack of funding and workforce shortages. 27 https://www.bbc.co.uk/news/health-65481473
So while the government claims that additional powers for pharmacists will reduce GPs’ workload, this measure is more accurately described as a shifting of demand from one (high profile) part of primary care to another, where it is more difficult to assess the impact of the change on staff or patients.
Until the government addresses the GP workforce crisis, it will remain difficult to get an appointment
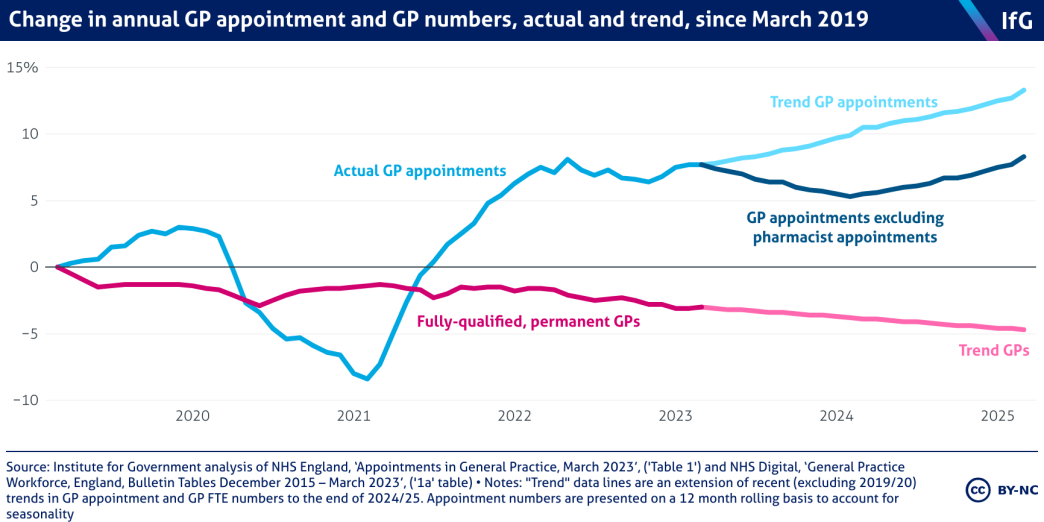
Despite the impressive increases in DPC staff, the number of fully-qualified, permanent GPs continues to decline. In March 2023, there were 823 fewer fully-qualified, permanent GPs than in the same month in 2019 – a 3% fall. In the same time, GPs delivered more appointments than ever: 162m in 2022/23 compared to 154m in 2019/20 – a 5.3% increase.
This increase comes with a cost. The higher workload has meant increased GP stress and burnout, with younger GPs leaving the service at record rates. As of now, there is no plan for how the government plans to increase GP numbers. The new “delivery plan” claims that “the NHS Long Term Workforce Plan […] will set out our ambitious plans to significantly expand GP specialty training and ensure the NHS can recruit and retain the GP workforce it needs in the future”, but it is unclear when that plan will be published and the Treasury is reportedly attempting to lower its commitments to higher workforce numbers. 28 https://www.theguardian.com/society/2023/mar/26/nhs-england-staff-shortages-could-exceed-570000-by-2036-study-finds
If trend increases in appointments persist, GPs will be expected to deliver the same number of appointments by March 2025 as they are now, even with 15 million appointments shifted to pharmacists. But if recent trends continue, there will be fewer fully-qualified, permanent GPs in March 2025 than in March 2023. This outcome is only likely to further worsen GP retention.
Against this backdrop, the government’s new plan to improve access to GP services could either be seen as an attempt to cover up falling GP numbers – by managing demand out of the system or onto less qualified colleagues – or as ineffectual tinkering at the edges. Improved telephone systems, triage and a rationalised targets regime are welcome, but they won’t deal with the serious workforce issues facing general practice.
- Topic
- Public services
- Political party
- Conservative
- Administration
- Sunak government
- Department
- Department of Health and Social Care
- Public figures
- Rishi Sunak
- Publisher
- Institute for Government